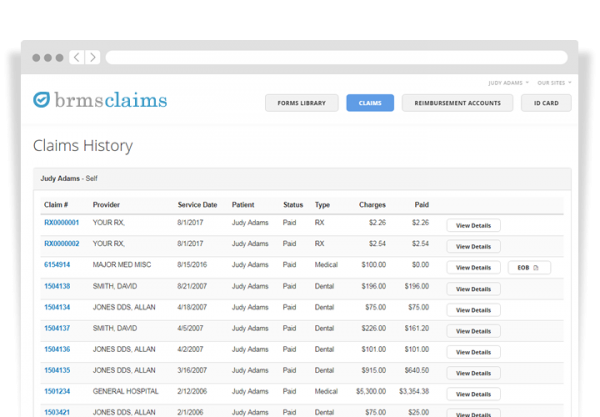
BRMS processes and manages all Medical, Dental, Vision and Retiree claims efficiently and accurately with an impeccable turnaround time. With eligibility transferred from our MyHealthBenefits system nightly, eligibility is completely current. And, with PPO negotiation expertise, we specialize in reducing employer claims costs.
Benefit Plan Administration
From receipt to eligibility to negotiation and payment, we handle the entire claims administration process. Completely centralized, all claims, medical management, PPO network management, and billing is managed in-house, allowing us to provide you with flexible and quick service with a personal touch.
For self-insured organizations, BRMS provides an excellent resource to process Medical, Dental and Vision claims efficiently and accurately.
TPA Auditing
We can audit claim activity for accuracy and reimburse recovered funds.
When you choose BRMS as your TPA, we can collect and review your previous TPA’s data, audit claim activity for accuracy, and reimburse recovered funds.
Claim procedure auditing on prior administrators determines compliance, assesses timeliness of claims payment, determines monetary penalties, evaluates accuracy of payments, and captures for potential fraudulent and abusive claim submissions, duplicates and other errors.
With risk management services that uncover, analyze and control potential losses due to unpredictable events, BRMS has a reputation for assisting companies in loss prevention and recovery.
Reporting and Data Analytics
BRMS’ reports identify trends in healthcare spending (a macro view) as well as opportunities for specific, member-level care improvement/cost avoidance (a micro view). We provide guidance for evaluating health plan performance, benefit planning, areas of cost avoidance, and clinical intervention opportunities.
Want to streamline your processes?
Contact us NOW to find out how we can help you save time and money by streamlining your Claims Administration!

